Osteochondritis Dissecan of the Knee
Cartilage is a semi-rigid, flexible connecting tissue surrounding joints. They envelop the ends of the bones and providing cushion-like support to joint bones. When there is loss of this construct this is called a Chondral Deffect. This is a painful condition and is the debility representing with different name in different condition. These can be a spectrum from single focal defect to advanced multifocal loss. It gets its nourishment from the synovial fluid supported by knee motion. It has poor blood supply. It is supported by underlying bone for this, thus the osteochondral unit makes it functional entity. Losing contact from underlying bone turn it non viable tissue. The condition Osteochondritis Dissecan is in which the unit lose its attachment from mother bone.
Osteochondritis dissecans can be split into
- juvenile form (JOCD),physes open age 4 -15 year
- adult form (skeletal maturity)
- location
- knee (most common)
- capitellum of humerus
- talus
Frequently in knee. This is a synovial joint where 3 bones: femur, tibia and patella articulate with each other. It consists of 2 articulations. The first is located between the femur and tibia. The femoral condyles (lateral and medial) which are the distal rounded ends of the femur, articulate with the proximal side of the tibia (tibia plateau). The second joint is the one between the femur and the patella.
There are two main places in the knee joint where osteochondritis dissecans can appear. One where mostly affects the femoral condyles, especially the medial condyle on the lateral joint surface (±70%). This area carries the least weight. 10% of the incidence is on the patella. OCD is more common in males and bilateral representation is rare (±25%).
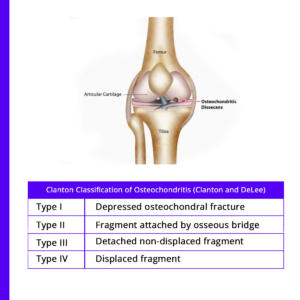
Path physiology -mechanism/etiology may be hereditary, traumatic, vascular
Prognosis
I. Juvenile form
A. Age.
i. younger the better the prognosis
ii. open distal femoral physes are the best predictor of successful non-operative management
B. Location -lesions in lateral femoral condyle and patella have poorer prognosis
C. Radiological predictors
1. sclerosis on x rays correlates with poor prognosis
2. synovial fluid behind the lesion on MRI correlates with a worse prognosis
II. Adult form
a) worse prognosis
b) symptomatic and leads to Degenerative Artheritis if left untreated.
When to see a doctor?
If you have persistent pain or soreness in your knee, elbow or another joint. This most common symptom of osteochondritis dissecans might be triggered by physical activity — walking up stairs, climbing a hill or playing sports, see your doctor.
Other signs and symptoms that should prompt a call or visit to your best knee specialist in Delhi or doctor in vicinity include joint swelling or inability to move a joint through its full range of motion.
Joint popping or locking –Your joint might pop or stick in one position if a loose fragment gets caught between bones during movement.
Joint weakness –You might feel as though your joint is “giving way” or weakening.
How is this managed by doctor?
1. Non operative – Plaster, splintage , rest and medication.
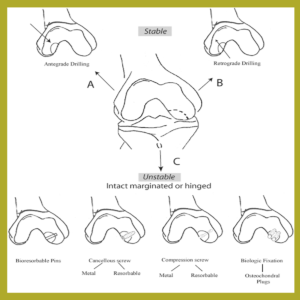
2 Operative – for severe cases,
• Removal of loose fragments
• fixation of the fragments with implants.
• Osteochondral autograft transplantation (OATS).
• Osteochondral allograft transplantation.
• Autologous chondrocyte implantation (ACI)
Prevention
Adolescents participating in organized sports might benefit from education on the risks to their joints associated with overuse. They should be under guidance of a good coach or paramedic. Learning the proper mechanics and techniques of their sport, using the proper protective gear, and participating in strength training and stability training exercises can help reduce the chance of injury. Early vigilant visit to your doctor if any such symptoms persist more than a day or two.
Contact Us
- Orthopedic clinic JMC Hospital, Joshi Rd, Block 63, Karol Bagh, New Delhi, Delhi 110005
- +91 8595471202
- drrajeshbhalla@yahoo.com
